Background of the Study
Female genital mutilation (FGM) is a procedure done to girls that involves removal of the labia majora and clitoris by cutting and sewing afterwards. Medically, it has no clear reason since it does more harm than good and creates social and psychological consequences to the girls who undergo the procedure (Leye, Van Eekert, Shamu, Esho, & Barrett 2019). FGM causes problems during childbirth. Midwives state that they have to give the parturients generous episiotomies and mothers had a slight risk for post-partum hemorrhage during caesarean sections (Balachandran, Duvalla, Sultan, & Thakar 2018). FGM practice is still being upheld in certain American communities, despite the dangers it exposes women to. Gender oppression is visible in disputing arguments that favor FGM practice (Wade 2017).
Globally, an effort to curb FGM practice, that has detrimental effects in millions of women and girls, has proved futile. This is because most perpetrators of the criminal act often go scot-free in many countries, without any punishment or prosecution. Moreover, change of laws is required to consider FGM as child abuse, which is hard to implement since it is hard to determine whether the girls are consented before the act (Couzens 2017). The prevalence of female genital mutilation has been estimated from large-scale national surveys asking women aged 15–49 years if they themselves or their daughters have been cut. Considerable variations have been found between countries, with prevalence rates over 80% in eight countries (UNICEF 2016).
The prevalence of FGM, attitudes towards it, and health consequences caused by FGM in Africa show that the practice is still accepted in the continent and practiced on girls at their younger ages in some villages. Over 130 million women and girls have experienced FGM in the 29 countries in which the practice is concentrated (Gruenbaum 2016). The highest incidence of FGM has been reported in Somalia, Djibouti, Eritrea, Sierra Leone, Sudan, Egypt, and Gambia. In some countries it is practiced more often in urban areas, while in some countries it is widely practiced in villages (Belda and Tololu 2017).
The procedure is typically carried out, with or without anesthesia, by a traditional circumciser using a knife or razor. The procedure involves removal of the clitoris, the inner and outer labia and closure of the vulva (Antia & Stinson 2015). The United Nations Population Fund estimates that 20 percent of women have been infibulated, a practice found largely in northeast Africa, particularly Djibouti, Eritrea, Somalia, and northern Sudan (UNFP 2015). Some studies investigating the experiences of girls who have undergone FGM and whether they liked or recommended it have been realized (Obiora, Maree, & Mafutha 2019). Slightly less than half of women are likely to undergo FGM in a city in Nigeria, and the possibility of passing the practice to younger generations was high. Age group, ethnicity, educational status, and knowledge of FGM were factors influencing the practice (Obi & Igbinadolor 2018).
In Kenya, the Northeastern province, followed by Eastern province, Nyanza and Rift Valley, have had more cases, while Central, Coast, Nairobi, and Western provinces recorded lower incidences. The practice is more common in rural than urban areas and most prevalent among women in the Somali, Samburu, Kisii and Maasai ethnic groups. Muslim women are more likely to experience FGM compared to other religious groups (Njonjo 2016).
It is possible to state that female genital mutilation has declined in Kenya, though some communities still practice it due to reasons related to culture, religion, social conditions and treating FGM as a rite of passage. Surprisingly, trained health workers performed the procedure in Abagusii, and Somali tribes and women reported complications and legal implications in the region (Kimani, Kabiru, Muteshi & Guy 2020). Cultural changes on perception of FGM practices among families and healthcare providers in some Kenyan tribes have led to increase in adaption of the out banned ritual. Firstly, the communities are initiating the cut to younger girls; secondly, they are making it a compulsory ritual before marriage (Kimani & Kabiru 2018).
In Kenya the practice of female mutilation is considered dangerous, and the country has imposed laws to prevent the practice from continuation. Evidence from the recently launched Kenya Demographic and Health Survey (KDHS) 2018 indicates that the overall prevalence of FGM has been decreasing over the last decade (Antia & Stinson 2018). In 2016, 27% of women had undergone FGM, a decline from 32% in 2014 and 38% in 2013. Older women are more likely to have undergone FGM than younger women, further indicating that the prevalence is decreasing. Moreover, the culture has remained highest among the Somali (91%), Kisii (89%), Kuria (90%) and the Masaai (92%) groups, while among the Kikuyu, Kamba, and Turkana groups it is least practiced, and rarely practiced among the Luo and Luhya (less than 1%). Therefore, it is against this background that the study seeks to find out the awareness of pregnant women on the health-related problems and how they influence the practice of female genital mutilation. The study was conducted among pregnant women in maternity wing, Dagahaley Médicins Sans Frontières Hospital, in Kenya.
Problem Statement
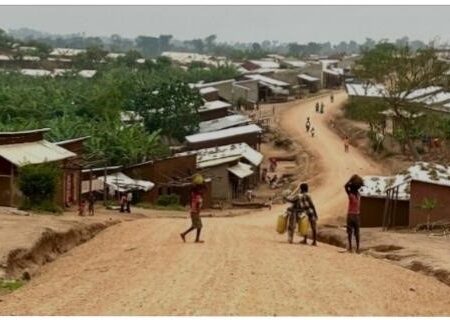
Female Genital Mutilation/Cutting is mostly done by traditional circumcisers, usually elderly women in the community, referred as traditional birth attendants. Cutting is done with special knives and razor blades. The practice is primarily found in areas with high rates of poverty, child mortality, illiteracy, poor sanitation, and difficulties to access modern health care facilities. Religion, tradition, and poor economic and social status of the women are among the most common factors reported to play a role for the practice to continue. Although the damage to female sexual organs and their function is extensive and irreversible, the true magnitude of the problem is still underestimated due to limited information about the practice. FGM is widely practiced by the Somali community, and it is one of the main causes for high maternal mortality. Approximately 90% of women and girls in Dagahaley refugee camp have undergone one form of FGC in their lifetime. The practice is considered as a major national problem, as it does not only affect the physical, mental, and social life of more than half of the Somali population, but also socio-economic development of the refugee camp. So far, the true magnitude of the problem and the nature of successful interventions is not yet known in Dagahaley. Moreover, rural Dagahaley is one of the potential regions of this practice. Hence this study aims to determine the knowledge and attitudes of women towards the practice. (UNICEF, 2016).
Dagahaley refugee camp is inhabited mostly by ethnic Somalis. Many young girls drop out of school after undergoing FGM and getting married. Traditional circumcisers and traditional birth attendants are mainly responsible for conducting the practice. They do not pay attention to infection control and sterility, thus exposing the girls to infections before the wounds heal and problems during childbirth due to narrowing birth canal. Currently, there are efforts to stop the practice by training volunteers as female FGM peer supporters, who provide emotional and practical support that enable women to seek help on their FGM-related health issues, and work alongside social workers to refer women to appropriate services for help and advice.
Table 1.1 Prevalence of FGM in Kenya among women and girls by age (%)
| Age group | 1998 | 2003 | 2008-2009 |
| 15-19 | 26.0 | 20.3 | 14.6 |
| 20-24 | 32.2 | 24.8 | 21.1 |
| 25-29 | 40.4 | 22.0 | 25.3 |
| 30-34 | 40.9 | 38.1 | 30.0 |
| 35-39 | 49.3 | 39.7 | 35.1 |
| 40-44 | 47.4 | 47.5 | 39.8 |
| 45-49 | 47.5 | 47.7 | 48.8 |
| Total | 37.6 | 32.3 | 27.1 |
Table 1.2 Prevalence of FGM by province and type in 2008
Research Questions
The research objective of this study is to assess the level of knowledge and attitudes towards the practice of female genital mutilation among pregnant women attending maternity wing at Dagahaley Médecins Sans Frontières Hospital. This is done by answering two research questions:
- What is the level of knowledge on the practice of female genital mutilation among pregnant women attending maternity wing in Dagahaley MSF Hospital?
- What are the attitudes towards the practice of female genital mutilation affect pregnant women attending maternity wing in Dagahaley MSF Hospital?
Justification and Significance of the Study
The World Health Organization has guidelines to combat FGM that highlight its health complications. The practice violates human rights since it is usually forced. Organizations working with populations practicing FGM have stressed the important role of health care providers in upholding health-related human rights of women and girls who are survivors of FGM or who are at risk of experiencing the procedure (Khosla, Banerjee, Chou, Say, & Fried 2017).
To offer effective health education to women on FGM practices, their socio-demographic and economic position, alongside traditions and beliefs need to be considered. This leads to a change in behavior and attitudes, which diminishes the probability of FGM (Waigwa, Doos, Bradbury-Jones & Taylor 2018). The idea that FGM practice should be stopped has gained visibility in recent years among women in Egypt, especially among non-circumcised women and wealthy, highly educated urban women (Van, Meekers & Gage 2016).
Studies done on FGM by the Kenya Demographic Health Services (2018) concerning ethnicity reveal that female genital cutting is prevalent among the Somali at 91% and the Kisii at 89%. Emerging factors and features from previous studies on FGM reflect the high level of ignorance among the community on children’s rights as described in the Children’s Act of 2001, and the negative impact that the procedure has on girls’ development and advancement. There has been a marked trend of girls undergoing FGM much younger than before, with many girls under 10 years of age. Although studies have been carried out to indicate the highly negative impact and consequences of FGM, they have not addressed reasons for the persistence of the practice. Therefore, a proper understanding of reasons behind the persistence of the practice is needed to achieve participation of women in development goals and improvement of women’s health. Despite the efforts directed towards decreasing the prevalence of FGM, the numbers remain high. As the efforts to control the practice are increasing, the ways of hiding it are becoming more discrete. This is an issue that requires an in-depth investigation into persistence of the practice.
Assessing the knowledge and attitudes of the main victims of FGM is an especially important measure towards the movement of discharging this long held tradition from a society which is suffering from its immediate as well long-term consequences. It has great significance in the preparation for creating an attitude change in mothers and empowering them by highlighting that most common reasons for FGM stem from direct or indirect attitudes of downgrading women and seeing them as beings created to serve the other sex. This social attitude plays an important role that needs to be changed to achieve behavioral change. Improvement of maternal health is incorporated to the sustainable development goals (SDGs) as one of the prerequisites for development and poverty reduction. Therefore, it is essential to describe the pregnant women’s knowledge and attitudes towards FGM before actions for improvement of maternal health. The study is significant and sociologically relevant because it provides insights into the knowledge and attitudes surrounding the persistence of FGM and its effects on girls, such as long term health problems. Moreover, FGM exposes women to greater risk of HIV. In other words, prohibiting FGM reduces health problems among women. The study will also contribute to the existing body of literature regarding the FGM. The study results will be used at all levels to play a part in the improvement of maternal health, ranging from healthcare planners to those working in the periphery. The study is also accessible for others who want to use the study results for their studies in related topics in the future.
Literature review
Government authorities have come up with plans against FGM as it is considered child abuse. However, there is little public effort to stop the practice (Christoffersen, Bruhn, de Neergaard, Engel & Naeser 2018). Training and updated clinical guidelines were suggested to correct the deficiency of information and help clinicians recognize, manage, and prevent FGM among children (Sureshkumar et al. 2016). To effectively combat FGM practice, replacing social cultures that support it is necessary (Klein, Helzner, Shayowitz, Kohlhoff & Smith-Norowitz 2018). Reig‐Alcaraz, Siles‐González & Solano‐Ruiz (2016) stated that there is lack of coordinated effort among clinicians to educate communities to stop FGM practice. The existing laws and health practices should support professional training to eradicate FGM, prevent FGM procedures, and support girls who have undergone the procedure (Reig‐Alcaraz, Siles‐González, & Solano‐Ruiz, 2016).
While any form of circumcision presents a danger to the women involved, the use of a method called pharaonic circumcision is particularly harmful. It involves cutting of the labia majora, labia minora and the clitoris, as well as both an external and internal stitching of the genitalia after the cutting process is completed (UNESCO 2015). A case study of Suardi et al., (2015) on young refugee victims of FGM asserts that FGM is generally performed by lay persons, including family members, often with non-sterile instruments and without anesthesia, analgesics, or antibiotics. FGM is also associated with substantial morbidity and medical complications that have been extensively documented (Yoder et al. 2014).
The definition of female genital mutilation states that it is a procedure done to girls that involves removal of the labia majora and clitoris by cutting and sewing afterwards (Leye, Van Eekert, Shamu, Esho & Barrett 2019). In his study, Gruenbaum (2016) found out that the majority of women knew what FGM is, they considered it as a form of gender-based violence and a human rights violation; further, because it is primarily perpetuated against young girls, it can also be considered a gendered form of child abuse. A study on how women perceived female genital mutilation revealed that the majority of women did not believe FGM to be a viable practice since it was illegal in the United Kingdom (Larsson, Cohen, Hann, Creighton & Hodes 2018). Furthermore, the women described the procedure as one in which some female genital parts were cut, and believed this could cause a lot of bleeding and danger to women who underwent the procedure.
In a study that evaluated rural residents’ knowledge on FGM-related complications showed that the majority of females knew that the practice severely affected girls’ health and welfare. Similar findings were reported by Moges et al. (2014) in a study conducted to assess knowledge of women towards FGM in Ethiopia. A study by Gruenbaum (2016) found a high level of knowledge regarding most of the complications of FGM, as more than half of respondents knew at least four complications of the procedure. Awareness on the global anti-FGM campaign was also high. The most common reasons for the practice of FGM were based on tradition or religion (Gruenbaum 2016). According to Hosken (2014), there was a significant increase in the proportion of respondents in Ethiopia who knew about FGM complications and who had no intention of circumcising girls in the future. Despite high level of knowledge regarding the complications of FGM and high level of awareness on the global campaign against it, the prevalence of FGM in this community was still high (Hosken, 2014).
A study done on effects of FGM have found out that circumcised women were 1.5 times more likely to experience pain during sexual intercourse, experience significantly less sexual satisfaction and were twice as likely to report that they did not experience sexual desire (Berg & Denison, 2017). A study by Belda & Tololu (2017) found out that rural residents’ knowledge on the consequences of FGM in Egypt was high, since most respondents stated it affected girls’ health and welfare. Moreover, the mothers also mentioned FGM could lead to health problems immediately during the procedure and childbirth.
Several countries, including Kenya, have developed laws and legislations banning the practice of FGM. A study done in Kisii indicates that there is a high level of awareness on laws concerning FGM as the majority of respondents knew about them. There are several legal instruments which seek to address the practice of FGM. Most respondents of the study in Kisii knew about the Anti-FGM law, the Children’s Act of 2001, and some about the Kenyan Constitution of 2010. Despite the knowledge of anti-FGM legal instruments, the majority of respondents indicated that they were not aware of any person having been punished for performing FGM (Eveline 2016). In a survey conducted in Sudan regarding public knowledge about the functions of female external genital organs showed that only about a third of respondents had sufficient knowledge (Richard, 2016). In Egypt, more than half of the rural residents knew that FGM was against the law (Mohammed, Seedhom and Mahfouz 2018).
Although the law in Kenya prohibits pharaonic circumcision, its practice among the Somali groups is still pervasive and encouraged by the local culture. There is extremely limited gender awareness and little knowledge on legal rights, especially those of children, among the Somali. Vested interests also serve to perpetuate the practice since it is a source of income for its practitioners, who are mostly specialized circumcisers, TBAs (traditional birth attendants) and midwives (Pracht 2017). Therefore, alternative sources of income are needed for the women who perform FGM. These women will then find they no longer need to rely on harming young girls for income and will eventually reject the practice (Lightfoot-Klein 2015).
While most countries have adopted legal frameworks prohibiting FGM, these measures have been ineffective in preventing and/or in accelerating the abandonment of the practice. Although evidence suggests legislation has not influenced the decline in FGM in many countries, legal frameworks are nevertheless key components of a comprehensive response to the elimination and abandonment of the practice.
Women undergo FGM due to personal and cultural beliefs (Abdulcadir, Say & Pallitto 2017). Personal awareness of available clinical guidelines and laws, caregiver’s confidence in management of women with FGM, communication and personal perceptions also supported the practice (Abdulcadir, Say, & Pallitto 2017). Majority of the women affected by FGM reside in the rural areas and have limited access to reproductive health education. As such, many myths about FGM have been passed down from generation to generation without being questioned and are subsequently held on to with tenacity (The FGM Programme 2019).
In most African countries, women with more education are less likely to have undergone FGM. Consequently, it is more likely that daughters of women who are highly educated are less likely to undergo FGM than daughters of women with little or no education (Yoder, Abderrahim & Zuzhuni 2014). A study by Sipsma et al., (2012), indicated that having less education was associated with higher odds of having had a daughter circumcised. Additionally, those with less education believed that FGM should continue. Findings from a study done in San Diego indicate that women who had undergone the procedure were clueless of why and for what reasons they underwent FGM (Hernandez, Hassan, Moalin, & Tidwell, 2018).
Hughes (2016) contrasts whether FGM is a matter of custom and tradition or an abuse of human rights. His argument is supportive of the World Health Organization’s (2016) view that female genital mutilation is a deeply rooted, traditional practice that has adverse physical and psychological consequences, in effect making FGM a form of violence against women. Traditionally, in many African and Middle Eastern cultures, circumcision was carried out by traditional birth attendants and circumcisers who were not medically trained, and though some medical professionals are still taking part in this practice, there has never been a medical reason identified for carrying out the procedure.
FGM is practiced because it is seen as a rite of passage from childhood to adulthood in some communities. The cultural significance of the practice is seen to be the preservation of chastity and to ensure marriageability of the girl child. The roots of the practice run deep into the individual’s psychology, sense of loyalty towards one’s family and belief in its value system (WHO 2015). In the study by Belda and Tololu (2017) in Ethiopia, majority of the mothers (96.9%) believed that FGM is a cultural practice. According to the Center for Reproductive Rights (2005), promotion of chastity and preventing promiscuity within the community were underpinning reasons for FGM. The patriarchal control over women and their sexuality, and ultimately their lack of access to resources, could perpetuate the practice of FGM (Monahan 2007).
Culturally, FGM is also associated with family honor, a vital attribute in certain communities. In these communities, a woman represents and retains her father’s lineage and marriage is seen as an alliance of two lineages. If a woman loses her honor, her entire family will be dishonored. Once the honor is lost, it cannot be restored and is particularly detrimental to the male figures in the family. Therefore, FGM is practiced to support and sustain honor (The FGM Programme 2019).
Girls’ and women’s beliefs on FGM vary widely across different countries. Despite some women advocating for FGM, most women in various studies believed the practice should be stopped and reported that they would not have their own daughters circumcised. The high proportion of the negative attitude towards the practice among young people may help to apply the social convention theory to increase knowledge among their parents about the harmful effects of FGM and prevent cutting their daughters in the future (Perron 2013; Kaplan et al. 2015; Yirga, 2016). A study among medical students in Egypt indicated that most female students had a favorable attitude towards discontinuation of the practice (Abolfotouh 2015).
The study by Mohammed (2016) in Iran, demonstrated that the majority of women felt that FGM did not make a woman feel happier or more accepted as a respectable woman. A review study in Nigeria had similar findings, demonstrating that female circumcision is not a religious requirement and did not change the behavior of women (Amusan 2015). Most respondents in the study considered the practice backward. The practice had outlived its usefulness, it had no tangible benefits, and promoted useless pride in the initiates. This indicated that attitudes towards FGM were changing, and women were had a positive attitude towards change of behavior. Similar findings were established in a study assessing the values associated with FGM that defined it as a tradition in transition (Berg & Denison 2017). This notwithstanding, in the Northeastern region of Kenya, a United Nations report noted that most women defended FGM and supported its continuation. Most refugee women of Somali origin living in Ethiopia also had a high intention to circumcise their daughters (Gebremariam 2017).
There are some values and beliefs that enhance the practice of FGM. These include beliefs that it enhances fertility, promotes purity, increases marriage opportunities, and prevents stillbirths. The values and beliefs are strongly rooted in tradition, culture, and religion, with no scientific basis (Sipsma et al. 2012). In many countries where FGM is practiced, traditional beliefs exist that an “uncircumcised woman” is unsuitable for marriage. Furthermore, there is a belief that FGM ensures a girl’s virginity, and that dowry is higher if a girl is a virgin at the time of marriage (Monahan 2007). Other beliefs that have fostered the practice of FGM include that the female genitalia are unclean and therefore the practice is necessary for hygiene; that the clitoris will continue to grow if not removed and start to resemble a penis between a woman’s legs; and that FGM, which removes the genitalia to control sexual behavior, can help control female desire and fidelity before and during marriage. There are parents who feel that their daughter will not be “normal”, socially acceptable, and marriageable if they do allow them to undergo FGM. The parents, who advocate for FGM, perceive it as a role that they should perform, so that they are not blamed by their daughters and society. They do not believe FGM is harmful, rather they are ensuring a safe and dignified place in society for their daughters (Monahan 2007).
According to Vercoutere (2020), most women perceived FGM as a good practice, with fewer seeing no reason for the practice. Reasons for the practice were traditional excitors who did not have good training, and parents of girls forcing them to circumcision without consulting or informing them about the practice. Most women stated they oppose the practice, as the law did not favor it and health-related risks were involved (Larsson, Cohen, Creighton, Hodes & Hann 2017). Parents and religious leaders did not support female circumcision because the practice compromised their daughters’ health (Abdulah, Dawson & Sedo,2020). Males perceived female circumcision as wickedness against females and stated it ought to be done away with. (Adeniran et al. 2016). The majority of women interviewed on effects of FGM were eager to abandon the practice after getting knowledge on its harmful and negative consequences on mental well-being and health. The health consequences cited by the women were painful childbirth, increased risk of female genital infection and use of unapproved medication to ease pain. Low self-esteem, disturbed body image and fear to have menses were some of the reported effects on the women’s mental well-being (Marcusán et al., 2016).
Religion has given the people impression that FGM is legal and acceptable according to what some religious leaders have stated. To stop FGM among those who practice for the sake of religion, religious leaders must take a firm stand of forbidding the practice. Otherwise, it will still be considered a requirement by religion, therefore, individuals and whole communities will continue to fulfill their religious duty despite its severe consequences (Dorkenoo 2016). FGM under the confident of religion is practiced in communities who commonly perceive it to be demanded as a religious obligation. Some religious scholars from Sudan believe both male and female circumcision is obligatory, and others encourage female excision as a preferable good deed (Suardi et al. 2015). This may have been initiated when Egypt’s prominent Islamic leader stated that FGM is an Islamic duty to which all Muslim women should adhere. Regions that are mostly Christian have the highest percentage of women affected by FGM (Boyle 2015). However, neither the Koran, which is the sacred Muslim text, nor the Bible has mention of FGM or a requirement to follow such traditions (Davis 2015). It will be difficult to convince believers of these communities to stop the practice of FGM without a strong stand by religious leaders (Dorkenoo 2016).
The perception of girls’ circumcision as an illegal practice is prevalent among men and women on an equal footing. In all parts of the world, women are facing threats to their lives, health, and wellbeing because of being overburdened with work combined to their lack of power and influence. In most regions of the world, women receive less formal education than men do, and at the same time, women’s own knowledge, abilities and coping mechanisms often go unrecognized (Eveline 2016).
Methodology
The study consisted of interviews on FGM practices with 15 pregnant women who were attending maternity wing of the Médecins Sans Frontières hospital. The researcher used oral history dialogue and a semi-structured questionnaire, which was used to collect information from the subjects as it allowed collection of more detailed information related to FGM practices. The questionnaire was both open- and close-ended. It was written in simple English that could be easily understood and was interpreted to Somali, since 90% of the respondents were not able to read English.
The study was carried out in a public health setting, hence the findings do not portray the situation among users of private antenatal clinics. To understand the situation of both public and private health facilities, further research needs to be conducted to compare findings and make recommendations.
The data was collected at Dagahaley Médecins Sans Frontières Hospital. Fifteen (15) questionnaires were issued, out of which 12 were confirmed to be accurate and complete with no particulars of the respondents written anywhere. They were analyzed to capture the objectives of this study.
Table 4.1 Social demographics of respondents
| Age group | 18 to 20 years | 3 |
| 21 to 25 years | 2 | |
| 26 to 30 years | 2 | |
| 31 to 35 years | 2 | |
| 36 to 40 years | 2 | |
| 41 years and above | 1 | |
| Total | 12 |
| Highest levels of education | No formal education | 7 |
| Primary | 3 | |
| Secondary | 1 | |
| Tertiary | 1 | |
| Total | 12 |
| Marital status | Married | 10 |
| Widow | 1 | |
| Divorced | 1 | |
| Total | 12 |
| Occupational status | Not employed | 8 |
| Employed | 2 | |
| Self-employed | 2 | |
| Total | 12 |
Knowledge on FGM practices
Majority of the respondents were knowledgeable on the definition of FGM. Most stated the definition to be a cultural rite of passage done to a girl once she attains a certain age. They stated that it is a practice done to remove the outer parts of the female reproductive system. A few respondents defined it as a religious practice that is done to preserve dignity and virginity of a woman until marriage.
Table 4.3 Knowledge on definition of FGM practice
| Knowledge on definition of FGM practice | ||
| Yes | 8 | |
| No | 4 | |
| Total | 12 | |
| Those who knew the definition | ||
| A cultural rite of passage done to a girl once she attains a certain age. | 8 | |
| A practice done to remove the outer parts of the female reproductive system. | 2 | |
| A religious practice that is done to preserve dignity and virginity of a woman till marriage. | 2 | |
Knowledge on effects of FGM
Only few of the respondents stated they knew the effects of FGM. Some stated severe pain as an effect of FGM, a few mentioned difficulty passing urine/feces, damage to urethra and difficult menstrual periods as immediate effects of FGM. Long-term effects of FGM that were mentioned were difficult childbirth, excessive bleeding (hemorrhage) and sexual dysfunctions.
Table 4.4 Knowledge on effects of FGM
| Knowledge on effects of FGM practice | ||
| Yes | 4 | |
| No | 8 | |
| Total | 12 | |
| Those who knew the effects | ||
| Immediate effects of FGM | ||
| Severe pain | 2 | |
| Difficulty passing urine/feces | 1 | |
| Damage of urethra | 2 | |
| Difficult menstrual periods | 1 | |
| Long term effects of FGM | ||
| Difficult childbirth | 2 | |
| Excessive bleeding (hemorrhage) | 1 | |
| Sexual dysfunction | 1 | |
Knowledge on laws
Majority of the respondents stated FGM was legal. Most of the respondents stated they were knowledgeable about the laws mentioned in the Koran, laws preventing child abuse and the Kenyan Constitution.
Table 4.5 Knowledge on laws on FGM practice
| Knowledge on laws of FGM practice | ||
| Yes | 10 | |
| No | 2 | |
| Total | 12 | |
| Those who knew the laws | ||
| Koran | 4 | |
| Prevention of child abuse law | 2 | |
| Kenyan Constitution | 2 | |
Knowledge on reasons for practicing FGM
Many respondents were not knowledgeable of why they practiced FGM. Less than half of the respondents stated as reasons for practicing FGM that it was a cultural rite of passage and that there were laws favoring it. Some stated poverty, benefits related to the practice, and school education as reasons for FGM.
Table 4.6 Reasons for practicing FGM
| Knowledge on reasons for practicing FGM practice. | ||
| Yes | 7 | |
| No | 5 | |
| Total | 12 | |
| Those who knew the reasons | ||
| Cultural rite of passage and laws favor | 3 | |
| Poverty | 1 | |
| Benefits | 2 | |
| Educated in school | 2 | |
Attitude towards FGM practices
Majority of the respondents believed FGM to be a compulsory cultural ritual. Most respondents strongly agreed or agreed FGM was a traditional and important practice. The respondents stated that FGM preserves girls’ chastity until marriage. Some stated it was a rite of passage, while for some the practice was associated with family honor. Few stated that the practice is necessary for hygiene since female genitalia are unclean. Some did not believe it prevented stillbirths or enhanced fertility. Most respondents also agreed that girls who had experienced it reported a lot of genital infections. A few respondents stated the practice had harmful and negative consequences on mental well-being and health. Some said FGM resulted in painful childbirth, while others stated the procedure caused low self-esteem, disturbed body image and fear to have menses. Less than half of respondents said that their community leaders had taken a firm stand of forbidding the practice and few had noticed that religious leaders would have convinced believers to forbid the practice. Few respondents knew that the practice is outlawed in the Kenyan constitution, while some noted that people in general perceive FGM as an illegal practice.
Conclusions
Knowledge about FGM, its definition and legal aspects related to the practice were known by pregnant women interviewed in the study. They were knowledgeable about the definition of FGM, laws concerning the practice and reasons against it. However, they were not knowledgeable on effects of FGM on their health.
Positive attitudes that supported FGM practice included seeing it as a cultural ritual, a traditional and important practice that preserved chastity until marriage. Negative attitudes that did not support the practice were known effects of FGM on women’s physical and mental health. FGM also caused low self-esteem and people perceived it as an illegal practice.
Recommendations based on this study:
- Maternity nurses ought to educate patients on FGM-related complications and its effects on maternal and fetal well-being during pregnancy and delivery as soon as the women arrive at the antenatal clinic.
- To change existing beliefs that support the practice, community healthcare nurses working with volunteers ought to organize weekly sessions to educate community leaders, who will in turn educate community members on how FGM has no known health benefits. Education is needed to take care of the health of women who have undergone FGM.
- To foster negative attitudes against FGM, the community law enforcers, who include chiefs and refugee block leaders working in collaboration with community heads, should ban the practice and act against those caught luring girls to FGM.
References
Abdulcadir, J., Say, L., & Pallitto, C. (2017). What do we know about assessing healthcare students and professionals’ knowledge, attitude and practice regarding female genital mutilation? A systematic review. Reproductive health, 14(1), 64.
Abdulah, D. M., Dawson, A., & Sedo, B. A. (2020). The impact of health education on attitudes of parents and religious leaders towards female genital mutilation. BMJ sexual & reproductive health, 46(1), 51-58.
Abolfotouh, A. Z., Ebrahim, K.J., & Abolfotouh, M. A. (2015). Awareness and predictors of female genital mutilation/cutting among young health advocates. International Journal of Women’s Health, vol. pp. 259–269.
Adeniran, A. S., Ijaiya, M. A., Fawole, A. A., Balogun, O. R., Adesina, K. T., Olatinwo, A. W. O., … & Adeniran, I. P. (2016). Attitudes to female genital mutilation/cutting among male adolescents in Ilorin, Nigeria. SAMJ: South African Medical Journal, 106(8), 822-823.
Alo, O. A., & Gbadebo, B. (2011). Intergenerational attitude changes regarding female genital cutting in Nigeria. Journal of Women’s Health, 20(11), 1655-1661.
Amusan O. A., & Asekun-Olarinmoye M. E. O. (2015). Knowledge, beliefs, and attitudes to female genital mutilation (FGM) in Shao Community of Kwara State, Nigeria. International Quarterly of Community Health Education. 27(4):337–348. doi: 10.2190/iq.27.4.e
Antia, S., & Stinson, M. (2015). Some conclusions on the education of deaf and hardof-hearing students in inclusive settings. Journal of Deaf Studies and Deaf Education, 4, 246-248
Asekun-Olarinmoye, E. O., & Amusan, O. A. (2008). The impact of health education on attitudes towards female genital mutilation (FGM) in a rural Nigerian community. The European Journal of Contraception & Reproductive Health Care, 13(3), 289-297.
Balachandran, A. A., Duvalla, S., Sultan, A. H., & Thakar, R. (2018). Are obstetric outcomes affected by female genital mutilation? International urogynecology journal, 29(3), 339-344.
Belda, S. S., and Tololu, A.K. (2017). Knowledge, attitude and practice of mothers towards female genital mutilation in Southwest Shoa zone, Oromia region, Ethiopia. MOJ Public Health, 6(2):279-286.
Berg, R. C., & Denison, E. (2012). Interventions to reduce the prevalence of female genital mutilation/cutting in African countries. Campbell systematic reviews, 8(1), 1-155.
Berg R. C., & Denison E. (2017). A tradition in transition: factors perpetuating and hindering the continuance of female genital mutilation/cutting (FGM/C) summarized in a systematic review. Health Care for Women International. 34(10):837–859. doi: 10.1080/073 99332.2012.721417.
Boyle, E.H. (2015). Female Genital Cutting: Cultural Conflict in the Global Community. Baltimore and London: The Johns Hopkins University Press.
Center for Reproductive Rights (2005). Legislation on Female Genital Mutilation in the United States, Briefing paper. Available online at: www. Reproductiverights.org. p.3
Christoffersen, G. M., Bruhn, P. J., de Neergaard, R., Engel, S., & Naeser, V. (2018). Mapping the lack of public initiative against female genital mutilation in Denmark. Reproductive health, 15(1), 59.
Couzens, M. (2017). The prosecution of female genital mutilation: a discussion of its implications for South Africa in the light of a recent Australian case. South African Law Journal, 134(1), 116-140.
Davis, D.S. (2015). Male and Female Genital Alteration: A collision course with the law? Health Matrix: Journal of Law-Medicine, 11: 487-570.
Dorkenoo, Efua. (2016). Cutting the Rose, Female Genital Mutilation: The Practice and its Prevention. London: Minority Rights Publications.
Everline, B. M. (2016). Factors Influencing the Practice of Female Genital Mutilation in Kenya: A Case Study of Gachuba Division, Nyamira County. Master of Arts Degree in Sociology (Rural Sociology and Community Development), University of Nairobi.
Fisher, A. A., Laing, J. E. & Strocker, J.E. (1998). Handbook for Family Planning Operations Research Design in Sampling. (2nd ed.). New York, Population Council.
Gebremariam, D., Assefa, F., & Weldegebreal, J. (2017). Prevalence and associated factors of female genital cutting among young adult females in Jigjiga district, eastern Ethiopia: a cross-sectional mixed study. International Journal of Women’s Health, vol. 8, pp. 357–365.
Gruenbaum, E. (2016). The cultural debate over female circumcision: the Sudanese are arguing this one out for themselves. Medical Anthropology Quarterly, 10(4), 455-475
Hernandez, J., Hassan, N., Moalin, U., & Tidwell, C. (2018). Understanding Female genital mutilation experiences to inform future health practices.
Hughes, F. P. (2016). The Hosken Report: Genital and Sexual Mutilation of Females, Fourth Revised Edition (Women’s International Network News: Lexington, MA, 2015) pages 114-115, 192-202, and 216-218.
Kaplan, M. P., Torán, M. J., Moreno, M. J., Fàbregas, C. & Munoz, O. (2015). Perception of primary health professionals about female genital mutilation: from healthcare to intercultural competence. BMC Health Services Research, vol. 9, article no. 11.
KDHS, (2018). Kenya Demographic and Health Survey 2018. National Council for Population and Development, Central Bureau of Statistics, and Macro International Inc, Calverton, Maryland, USA.
Kenya National Bureau of Statistics (KNBS). (2008/2009) Kenya Demographic and Health Survey 2008-09. Calverton, Maryland: KNBS: 158-160.
Khodary, Y., & Hamdy, N. (2019). FGM in Egypt between socio-cultural barriers and lack of political will. Journal of Aggression, Conflict and Peace Research.
Khosla, R., Banerjee, J., Chou, D., Say, L., & Fried, S. T. (2017). Gender equality and human rights approaches to female genital mutilation: a review of international human rights norms and standards. Reproductive health, 14(1), 59.
Kimani, S., & Kabiru, C. W. (2018). Shifts in female genital mutilation/cutting in Kenya: Perspectives of families and health care providers.
Kimani, S., Kabiru, C. W., Muteshi, J., & Guyo, J. (2020). Female genital mutilation/cutting: Emerging factors sustaining medicalization related changes in selected Kenyan communities. PLoS one, 15(3), e0228410.
Klein, E., Helzner, E., Shayowitz, M., Kohlhoff, S., & Smith-Norowitz, T. A. (2018). Female genital mutilation: health consequences and complications—a short literature review. Obstetrics and gynecology international, 2018.
Larsson, M., Cohen, P., Creighton, S. M., Hodes, D., & Hann, G. (2017). G64 An exploration of attitudes towards female genital mutilation/cutting (fgm/c) in men and women accessing fgm/c services.
Larsson, M., Cohen, P., Hann, G., Creighton, S. M., & Hodes, D. (2018). An exploration of attitudes towards female genital mutilation (FGM) in men and women accessing FGM clinical services in London: a pilot study. Journal of Obstetrics and Gynaecology, 38(7), 1005-1009.
Leye, E., Van Eekert, N., Shamu, S., Esho, T., & Barrett, H. (2019). Debating medicalization of Female Genital Mutilation/Cutting (FGM/C): learning from (policy) experiences across countries. Reproductive health, 16(1), 158.
Lightfoot H., Klein, D. & Hanny. P (2015). Prisoners of Ritual: An Odyssey into Female Circumcision in Africa. London: Harrington Park, Print.
Marcusán, A. K., Singla, L. R., Secka, D. M., Utzet, M., & Le Charles, M. A. (2016). Female genital mutilation/cutting changes and trends in knowledge, attitudes, and practices among health care professionals in the Gambia. International journal of women’s health, 8, 103.
Mishori, R., Ottenheimer, D., & Cassoobhoy, A. (2019, November). Female Genital Mutilation/Cutting (FGM/C) in the US after the Michigan Ruling. Now what? In APHA’s 2019 Annual Meeting and Expo (Nov. 2-Nov. 6). American Public Health Association.
Mohammed, E.S., Seedhom, A.E., and Mahfouz, E.M. (2018). Female genital mutilation: current awareness, believes and future intention in rural Egypt. Reproductive Health, 15(175):1-10.
Mohammed G. F., Hassan M. M., & Eyada M. M. (2016). Female genital mutilation/cutting: will it continue? Journal of Sexual Medicine. 11(11):2756–2763. doi: 10.1111/jsm.12655.
Monahan, K. (2007). Cultural Beliefs, Human Rights Violations, and Female Genital Cutting. Journal of Immigrant and Refugee Studies, 5(3):21-35.
Mugenda, O. M. & Mugenda, A. G. (2003). Research Methods.Quantitative & Qualitative SApproaches. Nairobi: Press African Center for Technology Studies (ACTS)
Njonjo, C. (2016). FGM and issues of gender and human rights of women in Momoh, C. (Ed) Female Genital Mutilation. United Kingdom: Raddiffe Publishing.
Nour, N.M. (2017). Female genital cutting: clinical and cultural guidelines. Obstet Gynecol Surv.59 (4):272–279.
Obi, A. I., & Igbinadolor, O. L. (2018). Prevalence of female genital mutilation and its determinants among pregnant women in Benin City, Nigeria. Journal of Community Medicine and Primary Health Care, 30(2), 12-21.
Obiora, O. L., Maree, J. E., & Mafutha, N. (2019). Female Genital Mutilation in Africa: Scoping the Landscape of Evidence. International Journal of Africa Nursing Sciences, 100189.
Olaitan, O. L. (2010). Knowledge of female genital cutting among parents in south west Nigeria. Translational Biomedicine, 1(2).
Ongong’a, J.J. (2016). Re-evaluation of African Traditional Women Education: Eastern and Southern Africa, Nairobi: Kenyatta University. Vol. IB, Berce basic Resource Centre.
Perron, V. Senikas, M. & Burnett, H.N. (2013). Female genital cutting. Journal of Obstetrics and Gynaecology Canada, vol. 35, no. 11, pp. 1028–1045.
Reig‐Alcaraz, M., Siles‐González, J., & Solano‐Ruiz, C. (2016). A mixed‐method synthesis of knowledge, experiences and attitudes of health professionals to Female Genital Mutilation. Journal of advanced nursing, 72(2), 245-260.
Richard A. (2016). On the modesty of women in Arab Muslim villages in the accommodation of tradition. American Anthropologist. 70:691.
Sipsma, H.L., Chen, P.G., Ofori-Atta, A., Ilozumba, U.O., Karfo, K., and Bradley, E.H. (2012). Female genital cutting: current practices and beliefs in western Africa. Bulletin of the World Health Organization, 90:120-127.
Suardi, F.K., Waritay, U.T., Toubia, Y., and Sanderson, L.P. (2015). Female Circumcision; It’s Persistence among the maasai of Kenya; M.A Thesis: Nairobi, University of Nairobi
Sureshkumar, P., Zurynski, Y., Moloney, S., Raman, S., Varol, N., & Elliott, E. J. (2016). Female genital mutilation: Survey of paediatricians’ knowledge, attitudes and practice. Child abuse & neglect, 55, 1-9.
Tantet, C., Aupiais, C., Bourdon, M., Sorge, F., Pagès, A., Levy, D., … & Faye, A. (2018). Female genital mutilation: an evaluation of the knowledge of French general and specialized travel medicine practitioners. Journal of travel medicine, 25(1), tax090.
The FGM Programme, (2019). FGM in New Zealand. Beliefs and Issues sustaining the practice. Available from https://fgm.co.nz/background-to-fgm/believes-issues/
Toubia, N.A. (2015). A Practical Manual for Health Care Providers Caring for Women with Circumcision. New York: RAINBO Publication.
Turkmani, S., Homer, C., Varol, N., & Dawson, A. (2018). A survey of Australian midwives’ knowledge, experience, and training needs in relation to female genital mutilation. Women and Birth, 31(1), 25-30.
UNDP/UNFPA/WHO/World Bank Special Programme of Research, Development and Research Training in Human Reproduction. (2014). Dynamics of decision-making and change in the practice of female genital mutilation in the Gambia and Senegal: social science policy brief. Available from: http://www.who.int/reproductivehealth/publications/fgm/rhr hrp_10_16/en/. Accessed March 13, 2019.
Van, R. R., Meekers, D., & Gage, A. J. (2016). Trends in attitudes towards female genital mutilation among ever-married Egyptian women, evidence from the Demographic and Health Surveys, 1995-2014: paths of change. International journal for equity in health, 15, 31-31.
Vercoutere, A. (2020). 6. Beliefs and attitudes regarding FGM in a rural village in Region Kankan, Guinea, before the start of an awareness campaign. Journal of Obstetrics and Gynaecology Canada, 42(2), e19-e20.
Wade, L. (2017). Defining Gendered Oppression in US Newspapers: The Strategic Value of “Female Genital Mutilation”.
Waigwa, S., Doos, L., Bradbury-Jones, C., & Taylor, J. (2018). Effectiveness of health education as an intervention designed to prevent female genital mutilation/cutting (FGM/C): a systematic review. Reproductive health, 15(1), 62.
World Bank Report on FGM. (2015). Female Genital Mutilation/Cutting: A Statistical Exploration. New York: Oxford University press
Yader, A. M. Abderrahim, J., & Zhuzhuni, H. (2014). Working to End Female Genital Mutilation and Cutting in Tanzania: The Role and Response of the Church. Christian Council of Tanzania.Tanzania: 28 too Many.
Yirga, N. A., Kassa, M. W., Gebremichael, A. R. & Aro, W. S. (2016). Female genital mutilation: prevalence, perceptions and effect on women’s health in Kersa district of Ethiopia. International Journal of Women’s Health, vol. 4, no. 1, pp. 45–54.







Mohamed Omar Othowa have you thought to publish this work in a journal? This work is not only very well done but due to your positionality in the research it is really valuable work and it would be great if the information could go even wider.
Also, is this your graphic memoir? 😀 https://www.npr.org/sections/goatsandsoda/2021/10/16/1044055476/a-refugee-at-4-he-felt-like-a-lost-star-now-his-voice-shines-in-a-graphic-memoir?t=1645486029589