Coronavirus disease (Covid-19) first appeared in November 2019 in Wuhan, Hubei, China. It was declared a pandemic by the World Health Organization (WHO) on March 11th, 2020. As for September 19th, 2020, the registered cases across the globe were over 30 million, with almost 1 million confirmed deaths, and affecting a total of 216 countries. [1]
The main symptoms linked to Covid-19 are cold-like: fever, cough, tiredness, nasal congestion and headache. Other less common symptoms are diarrhea and loss of taste or smell. [1]
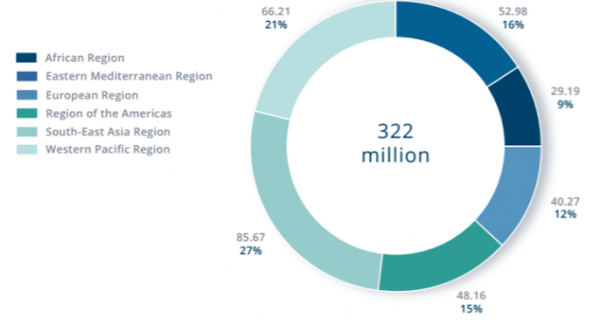
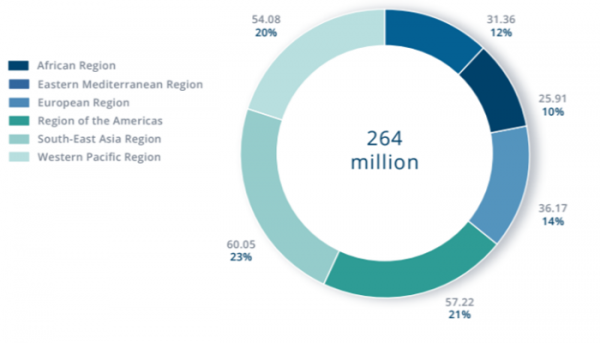
On the other hand, mental health illnesses such as depression and anxiety were already amongst the most prevalent diseases worldwide prior to the appearance of Covid-19. Depression affects 322 million people worldwide (4.4% of global population), whereas anxiety affects 264 million people worldwide (3.6% of global population) [2].
Some studies are starting to link Covid-19 with mental health disorders, especially the two previously mentioned. A study carried on Covid-19 survivors showed that a significant proportion of patients were suffering from some psychopathology, such as PTSD (28%), depression (31%), anxiety (42%), obsessive-compulsive symptoms (20%) and insomnia (40%) [3].
Other studies performed on the general public (not having suffered from Covid-19) showed a prevalence of anxiety of 35%, depressive symptoms of 20% and poor sleep quality of 18,2%, which indicates that both healthy and ill people are experiencing a deep impact of the pandemic in terms of mental health symptoms [2].
Furthermore, considering the effect depending on social groups, younger people experience greater rates of depressive symptoms, whereas healthcare workers experience a deeper impact of insomnia. Moreover, a greater exposure to Covid-19 information and more time spent worrying about Covid-19, have been linked to a greater chance of developing some of these symptoms [2]. In general terms, over information, quarantine, fear and the consequences of the economic crisis impact as well on mental health of overall population.
Focusing on the place where the interviews took place, it is important to understand de specific context of the pandemic in Spain. It is the 9th country in the world with most cases, with 640.040 confirmed cases and 30.500 confirmed deaths (updated September 19th) [1]. The measures regarding social distancing and quarantine have a deep impact in the Spanish way of being, very rooted in its familiar and social culture, where physical contact and social gatherings are an essential part of day-to-day life.
Besides, Spain is one of the most affected countries by the economic crises surging from the pandemic. One of the main reasons is its high dependency on tourism, being the first country in the OCDE in terms of percentage of the GDP coming from this sector of activity (12%) [3]. It has as well one the greatest unemployment rates, with an overall rate of 16%, and 41% for people under 25 years old [4]. Lastly, the impact of this economic crises has had a direct impact on Spain’s GDP, which is expected to drop around 20% compared to last year’s [5].
In this context of the Covid-19 pandemic, the prior impact of anxiety and depression and the situation in Spain, the interviews were arranged with people who had been infected with the virus.
The questions asked were the following:
- When were you sick with Covid-19?
- How did it affect you physically and psychologically?
- How long were you affected by it?
- Did you experience any anxiety or depression symptoms?
- Did your doctor mention the possibility of suffering any of these symptoms?
- How long did it take for you to fully recover?
- How would you describe the impact it had on you and your closest ones?
The three different interviewees or group of interviewees provided the answers as a narrative of their whole experience during their illness. The main information extracted is summarized here below:
- Interviewee 1: 21 years old male affected in March 2020. His condition lasted for 2 weeks in the acute phase, although it took him 2 months to fully recover. His physical symptoms were high fever, body ache and headaches.
- In terms of feelings, he experienced negativity related to the extreme fatigue, considering that he is a very sportive and active person and the complete absence of energy did not allow to do anything other than laying on the couch. This generated an overall feeling of discouragement, which produced frustration and irritability.
- Interviewee 2: 28 years old male affected in September 2020. His physical symptoms lasted for 2 weeks and they consisted of fever, diarrhea and gastritis, loss of appetite and loss of smell and taste.
- Psychologically, he experienced feelings of sadness for being alone and not being able to rely on his family and friends at a time of sickness and fear, as he would have usually done. This resulted in a severe anxiety experimented for several days with multiple panic attacks related to the possibility of developing more severe symptoms, generated by all of the information he had been following on the news during the whole pandemic; frustration related to lack of recovery, especially when he had been medicated for a whole week and he still had low fever at least once a day; and the confinement, which had him locked up in a small room with not much to do to entertain himself (there was no TV, he had no energy to read nor work). This whole situation was aggravated because of the fear of passing the virus to his girlfriend who lives with him and who had not caught the infection.
- Interviewee 3: this third interview was of a family of three affected at the same time in September 2020: a 23 years old female (the daughter), 54 years old female (the mother), and a 54 years old male (the father). The mother and daughter experienced mild symptoms such as fever, headaches and fatigue. However, the father experienced more severe symptoms. As he had been hospitalized prior to an intervention unrelated to Covid-19, when he started developing symptoms he got tested. When the results were positive, he was not allowed to return home because of his multiple sclerosis, that made him a risk patient with lower defenses against the virus. He then started to develop more severe symptoms, such as high fever that would not remit for eight consecutive days, bad cough and hypoxia, which made it necessary for him to be on oxygen. He was discharged after ten days of hospitalization.
- Psychologically, all of them experienced feelings of fear of infecting others once they could go out (this was aggravated because in Spain the second test is not provided by the National Health System, and you are discharged simply after two weeks since the beginning of the symptoms without knowing whether you are still contagious with a positive PCR); during the days of the illness, they had fear of developing more severe symptoms, especially regarding the father; also, they felt like this situation made them aware of the danger of the virus, which, up to that moment, they had only heard of but not experienced in their close environment. Finally, what they were feeling was an overall discouragement due to the confinement that reminded them of the three months that they had been locked up.
- It is important to note that both parents had depression-like symptoms: unwillingness to get out of bed and do anything more related to discouragement than to fatigue, and that lasted long after the symptoms had disappeared; lack of motivation and fatigue; irritation and change in humor, especially for the father; frustration related to lack of recovery, since two weeks after the beginning of the virus the two parents were still unwell with many of the symptoms still going on.
After the scientific research regarding the situation of Covid-19, anxiety and depression, and their interrelation, I found very interesting how everyone in my environment who had suffered this experience had indeed experienced this type of symptoms as well. However, until asked by me, they did not count them as symptoms of the infection and would simply not talk about them.
What I have been able to conclude is that, without a doubt, the Covid-10 virus has a negative impact on patient’s psychological state. However, it is unclear the exact way in which it affects us. The mental consequences may be produced because of the virus itself, as a direct impact on the brain system the same way it attacks the respiratory or gastrointestinal system. However, it may also be produced because of the confinement associated to being infected, plus the over-information everywhere that makes people think about the pandemic all the time. With Covid-19, there is a general awareness of the severity and possible fatality of the virus that does not occur with the usual illnesses we suffer from. Prior to 2020, did you know the fatality rate of the flu in your country? Because I most certainly did not. However, I can tell you the variations of the fatality rate of Covid-19 depending on the country, the testing volume and even by age groups.
Another interesting point that is being noticed by researchers, is that the virus affects the patient’s weakest points. If the patient tends to feel depressed or anxious, Covid-19 may exacerbate it.
However, what I find most concerning is the deep psychological impact this pandemic is having on the general population, related to the constant presence of Covid-19 on the news, the fear of being infected or infecting others, the uncertainty that surrounds us and that has flipped our society and our way of being upside down, the economic crisis produced by the drastic drop of tourism worldwide and the total lock down of the cities, the lack of freedom that we had never experienced until now.
To conclude, the sociological, psychological and sanitary consequences of the pandemic are still unknown. There is a mixture of the social context worldwide and the effects of the virus itself that are adding up to affect everyone in a different way, but producing an overall effect of anxiety, depression and insomnia.
I would like to finish by explaining how this topic is connected to border-crossing and global history.
First of all, this pandemic is one of the most impacting historical events we have experienced in the last decades. The hyper globalization has spread the virus through the whole globe, and although in the beginning we tended to compare it to the Spanish flu occurring in the beginning of the 20th century, the characteristics of our modern society have made the impact and consequences of Covid-19 completely different to those of the Spanish flu.
Secondly, this event is global because Covid-19 has started one of the deepest economic crises in modern society, due to a construction of our economic system based on international commerce and globalized supply chains. In January, when only China was locked down, the rest of the world’s economy was already being affected because of all the commerce agreements tht begin or end in China. There was later on, when the rest of the world was affected, a general need for face masks and breathing equipment, with some frictions beginning to happen between countries on their efforts to cover their own demand.
Finally, I would like to remark that prior to Covid-19, depression and anxiety were becoming a pandemic by themselves. Moreover, the sociological impacts of the pandemic (isolation, quarantine, uncertainty, unemployment) are increasing this problem worldwide. If we consider the difficulty to predict the long-term consequences of the pandemic in general, due to the complete uniqueness of this situation, it could happen that the rates of depression, anxiety and suicide skyrocket worldwide if there is not an appropriate response and approach to it.
Bibliography
| [1] | World Health Organization, «Coronavirus disease (COVID-19) pandemic,» 09 2020. [En línea]. Available: https://www.who.int/emergencies/diseases/novel-coronavirus-2019. [Último acceso: 19 09 2020]. |
| [2] | H. Yeen y Z. Ning, «Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey.,» Psychiatry Research, vol. 288, 2020. |
| [3] | M. Gennaro Mazzaa, R. De Lorenzob, C. Conteb y S. Polettia, «Anxiety and depression in COVID-19 survivors: Role of inflammatory and clinical predictors,» Brain, Behavior, and Immunity, 2020. |